Pancreatic and Gastric Cancer Awareness: Understanding the Signs and Risks
Clinically reviewed by Kim Bui, MD

Pancreatic and Gastric Cancers affect the gastro-intestinal (GI) system. In addition to the Pancreas and Stomach, the GI system also includes the Liver, Small and Large Bowel, and Rectum.1
Compared to other cancers, gastro-intestinal cancers have the highest rates of new diagnoses and account for 1 out of 4 cancer related deaths.2 GI cancers are a particular concern for individuals who identify as Asian American and Pacific Islander (AAPI). Despite relatively low cancer mortality overall, AAPI individuals diagnosed with liver or stomach cancer are 40-50% more likely to die from these cancers than white patients.3
The Charles B. Wang Community Health Center continues to encourage all to learn more about Pancreatic and Gastric cancers and start conversations with your healthcare providers and loved ones. Early awareness and early detection can make a difference!
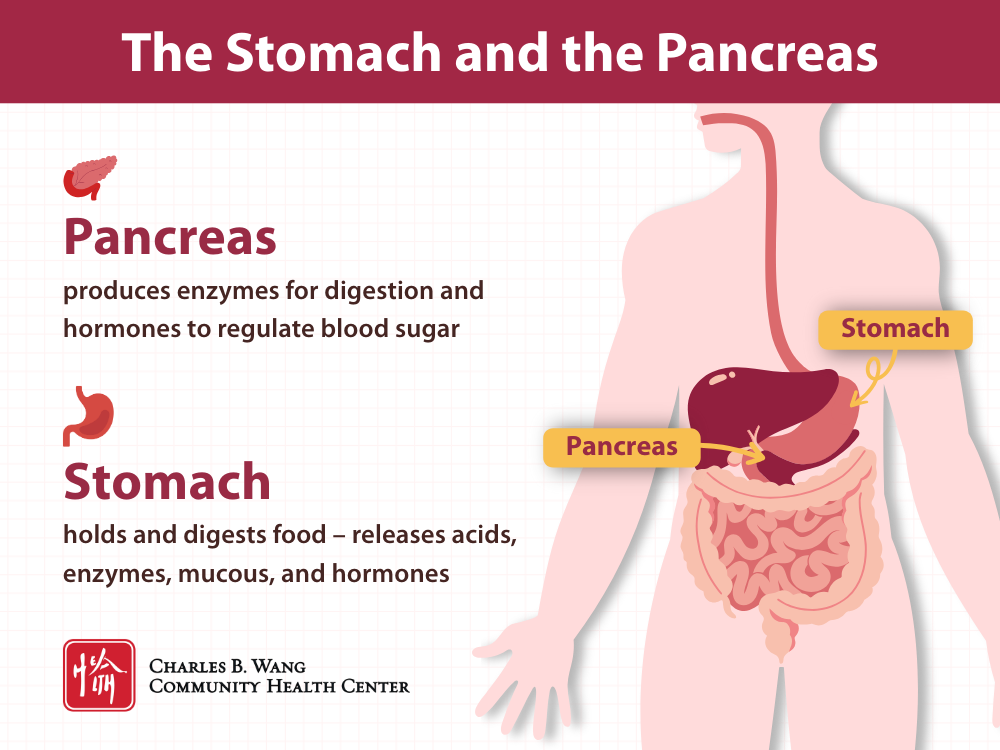
Understanding the Stomach and the Pancreas
To better understand how pancreatic and gastric cancers may impact the body, let’s start by getting a better understanding of what the stomach and the pancreas do.
The Stomach
The stomach is an organ that holds and digests food. The stomach is not very big, but it does have five sections and five layers of tissue (mucosa, submucosa, muscle layers, subserosa, and serosa). The mucosa layer is the inner most layer of the stomach which contains many glands that produce fluids, stomach acid, enzymes, and more. The stomach’s glands, nerves, and muscles work together to break down food, prepare the body to absorb energy and nutrients from food, and keep digestion moving from the esophagus to the intestines.4,5
The Pancreas
The pancreas is a gland that produces enzymes that support digestion and hormones that regulate blood sugar levels. Enzymes support digestion of the fats, carbohydrates, and proteins that we eat. Hormones like insulin and glucagon work as opposing signals to the liver, keeping blood sugar stable and providing the body with steady energy - insulin lowers blood sugar when it rises, while glucagon raises sugar when it falls.6,7
Pancreatic and Gastric Cancers
About Cancer
Our bodies are made up of many types of cells- like nerve cells, skin cells, and the pancreatic cells that make insulin. When our cells are growing and functioning normally, we feel healthy and well.
Cancer develops when there is a mutation in the normal DNA, which leads to abnormal growth of any of these normally well-functioning cells. Cancer cells grow or multiply without following the regular checks and balances in the body, they take resources away from neighboring cells, can cause bleeding or clotting, and eventually can spread to other parts of the body.8,9
Pancreatic and gastric cancers are more treatable when found early, but recognizing the signs and symptoms can be challenging. Learn more about the signs of pancreatic and gastric cancers to best advocate for the health of yourself, your loved ones, and your community.2,8,9
Gastric Cancer
Gastric carcinoma or cancer is a cancer that occurs in the stomach. The most common gastric cancers are adenocarcinomas that start in the innermost layer of the stomach (the mucosa) and affect the cells that produce our gastric juices.5,9
Common Signs of Gastric Cancer
Unfortunately, gastric cancer is often diagnosed at a late stage because many symptoms overlap with other more benign GI issues like heartburn. Weight loss and abdominal pain are the most common presenting symptoms. Additional signs include:
- ongoing indigestion or bloating
- feeling full quickly or not feeling hungry
- persistent heartburn
- fatigue
- blood in stool or vomiting (with or without blood)10
Pancreatic Cancer
Pancreatic carcinoma or cancer, is a cancer that occurs in the pancreas. Pancreatic ductal adenocarcinoma (PDAC) is an aggressive cancer accounting for over 90% of pancreatic neoplasms.6,11,12
Common Signs of Pancreatic Cancer
Like gastric cancer, pancreatic cancers are diagnosed at advanced stages because their symptoms overlap with many other GI diseases. Painless jaundice (yellowing of the skin or eyes) is more predictive of pancreatic cancer than other symptoms which include the following:
- belly pain or back pain
- unexplained weight loss or loss of appetite
- fatigue or abnormal weakness
- nausea and vomiting
- abrupt, new-onset, or dramatically worsening diabetes without a clear cause13,14
Pancreatic and Gastric Cancer Risks
Understanding the risks of pancreatic and stomach cancers can help you know your own personal risk, make changes where possible, and help inform your conversation about appropriate screening with your doctor.
Some risks are inherited or hard to change. Others can be managed through medical treatment or lifestyle changes. If you want to know more about your personal risk, talk with your healthcare provider.
Risk Factors That Can Be Addressed
Tobacco Use
Smoking tobacco is a significant risk factor for many types of cancers, including pancreatic and gastric cancers.15,16,17,18 Smoking doubles your risk for stomach cancer.16 Among patients with pancreatic cancer, it is estimated that 1 in 4 was caused by cigarette smoking.17
In New York City, about 1 in 5 AAPI men who were born outside of the US smoked in 2020.19 Nicotine is very addictive, but treatment and support are available. At the Charles B. Wang Community Health Center, our Certified Tobacco Treatment Specialists provide free in-person and phone counseling in English, Mandarin, and Cantonese as well as free medication therapies like Nicotine Replacement Therapy (NRT).
Alcohol Use
Alcohol use is also linked to increased risk of pancreatic and stomach cancers.17,18,19 People who drink 3 or more drinks per day may have a higher risk of pancreatic and gastric cancers.19 Heavy alcohol use may also lead to the development of other GI conditions like chronic pancreatitis, which can increase cancer risk.17 More research is being done to better understand the exact connections.
If you would like to stop or reduce your alcohol use, talking to your primary care provider (PCP) can be a great first step. Your provider can discuss possible treatments and help you create a plan that is aligned with your goals. You may also consider talking to a substance abuse counselor or joining a support program like a 12-step program or another peer support program.
Diet
Diets that are low in vegetables and fruit, and high in red and processed meat or foods preserved with salt, are linked to increased risk of pancreatic and gastric cancers.16,17,18,20 In general, a balanced diet full of a variety of whole grains, fruits, vegetables, nuts, seeds, and fish, can lower cancer risks.21 For GI cancers, eating fresh fruits, particularly citrus fruits, and raw vegetables may lower a person’s risk.16
When thinking about making changes to your diet, it can be helpful to think about small changes that help you find balance and variety. While cutting or adding a whole food group may be an overwhelming change, small changes can add up to reduce your risks. Small changes might look like: having a whole orange instead of orange juice, adding beans to soup instead of beef, choosing a whole grain rice variety like brown rice, red rice, or purple rice, or having a side of lightly salted cucumber instead of pickled vegetables.
Resources may also be available to supplement your family’s food budget. Food banks, free school meals, and community fridges can help your family meet your diet goals. There are many food assistance options available in NYC, The New York Public Library maintains a list of resources that are available for people of all ages, that may accommodate your dietary needs, and are accessible across all five boroughs and beyond.22
Helicobacter Pylori (H. pylori) Infection
H. pylori infection can cause stomach cancer, though most people with the infection do not develop cancer.16,23Tobacco use may compound a person’s risk of developing stomach cancer if they have H. pylori, while treatment of the infection can lower that risk.20,23,24H. pylori may be linked to pancreatic cancer but the evidence is less clear.17
H. pylori is common in many Asian countries.23,25,26,27 In the U.S., H. pylori is prevalent among East Asian immigrants, particularly among individuals who were born in Fujian province.24,25,26,27,28
H. pylori can cause abdominal pain, gastritis, ulcers, and heartburn. If you are concerned you may have the infection, talk to your primary care provider.23,24,28
Gum Disease
Individuals with poor dental health have a higher risk of both pancreatic and gastric cancers.18,29,30For stomach cancer in particular, tooth loss may be a significant risk factor.18,29,30
Caring for dental health is an important part of overall health. While it may not be a direct causal link, maintaining dental health may help reduce cancer risks. And for those suffering from gum disease, studies have found that treatment may also reduce cancer risk.31 At the Charles B. Wang Community Health Center our dental care team can support your dental health. Whether it has been 6 months or many years, it is never too late to start regular dental visits.
Other Risk Factors to Be Aware of
Chemical Exposure
Exposures to certain chemicals and heavy metals can increase pancreatic and gastric cancer risks.16,17,18,20 Chemicals that may increase a person's risk of pancreatic cancer include: asbestos, benzene, or pesticides.18 Individuals may be exposed to these chemicals in their homes, the environment, or at work. Individuals who have worked in the rubber or coal industries may have a higher risk of gastric cancer.16,20
Family History
Pancreatic and gastric cancers are more likely to occur among those who have a first-degree relative who has had pancreatic or gastric cancers.16,17,18,20Other inherited disorders may increase the likelihood of pancreatic or gastric cancers, like: Familial Adenomatous Polyposis (FAP), Hereditary Nonpolyposis Colorectal Cancer (HNPCC) or Lynch Syndrome, and Peutz-Jeghers Syndrome.16,17,18,20
Diabetes
New onset diabetes is a significant risk factor for pancreatic cancer.17,18
Age
Pancreatic and gastric cancer risks increase as a person gets older.16,17,18,20 Most pancreatic or gastric cancers are diagnosed after age 45. Stomach cancers are most commonly diagnosed during a person’s 60s-80s and the average age for a pancreatic cancer diagnoses is 70 years old.16,17
Sex
Pancreatic and gastric cancers are slightly more common among those who are assigned male at birth.16,17,18,20,32 The reason for this variation is not known with certainty, although connections between sex and rates of other risk factors like tobacco use may play a role.17,32
Talking about Pancreatic and Gastric Cancers
Treatment and health outcomes improve when pancreatic and gastric cancers are caught early. Use this knowledge to pay attention to changes and symptoms in your body and seek medical advice early.
Talk to Your Family About Risks
Understanding your family health history is an important component of your overall health. While conversations around cancer or digestion may be particularly uncomfortable, it is a critical starting point for recognizing your unique risks, advocating for your own health, and supporting the health of your family.
Talk to Your Provider About Pancreatic and Gastric Cancers
Talking to your primary care provider about your unique risks can be a good place to start.
For those with minimal or average risk, screenings for pancreatic or gastric cancers are not recommended.33,34 However, patients at high risk for these cancers may be eligible for screening with ultrasound or MRIs.33,34
Learn More with CBWCHC
Charles B. Wang Community Health Center provides primary care services that support your whole health. If you are looking to reduce your risks of pancreatic and gastric cancers, our internal medicine providers, dental health providers, and certified tobacco treatment specialists can support your health goals in a language you prefer.
Annual check-ups are a great time to talk with your primary care provider about your unique risk, medical history, and family history. Your primary care provider is also a great resource for connecting with a GI specialists, they may even be able to provide a recommendation. Internal Medicine providers at Charles B. Wang Community Health Center are available for appointments 7 days a week in Manhattan and Queens. Find an Internal Medicine provider or call (212) 379-6998 for Manhattan or (718) 587-1111 for Flushing to schedule your annual check-up today.
FAQs
1. Why are GI cancers often found at later stages than other cancers?
Since symptoms don’t usually develop right away and early symptoms overlap with many other common GI conditions like stomach ulcers; GI cancers like Pancreatic, Gastric, and Colorectal Cancers are often diagnosed later than other cancers. Additionally, in the U.S., patients at average risk are not screened for pancreatic and gastric cancers.33,34
2. Where can I learn more about what to do if I or someone I know has been diagnosed with pancreatic and gastric cancer?
You can learn more about cancer from your PCP, a cancer specialist, or other medical resources. The American Cancer Society maintains some resources for individuals impacted by cancer across the spectrum: from a 24/7 cancer helpline to caregiver support video series, this can be a good resource for those seeking support.35
A cancer diagnosis can be overwhelming. Make sure to make some time to care for yourself. Whether you are coping with news about a loved one or processing your own diagnosis, your ongoing well-being is important. Consider the level of self-care that makes sense for you, you might focus on: small moments of self-care (like taking time for a creative project), connecting with a peer support group, or talking to a mental health professional.35,36,37
3. How do health disparities impact cancer risk?
Due to a combination of social and environmental factors, health disparities exist. These health disparities become evident when we look at populations as a whole. While each person’s experience and likelihood of getting cancer is different, in general, a persons risk of being diagnosed with cancer or being diagnosed with later stage cancer may be higher due to their race or ethnicity.
- GI cancers including Liver Cancers, Colorectal Cancers, and Stomach Cancers are some of the most common cancers among individuals who identify as AANHPI.3
- Stomach cancer is the fourth most common cancer among Korean and Samoan men.3
- AAPI women, AIAN women, Hispanic women, and Black women are all over 2 times more likely to be diagnosed with stomach cancer than non-Hispanic white women.38
- Black Americans have the highest rates of new pancreatic cancer diagnoses in the US and are also more likely to be diagnosed with later stage pancreatic cancer.18,38,39
- A family’s immigration history may also play a role in their risk of cancer, particularly stomach cancer.25,40 Some studies have found that first and second-generation immigrants from countries with high rates of stomach cancer have a higher risk of stomach cancer compared to others in their country of residence, even after immigrating.26 Individuals who have immigrated to the U.S. from Eastern Asia and Eastern Europe have been shown to have higher rates of new stomach cancer diagnoses.40
4. How can I start the conversation about GI cancers with my family?
It may be helpful to create a plan for how you will start the conversation, support your loved ones, and get your questions answered.41,42
You might first consider where and when to have the conversation. As difficult as the conversation might be for you to start, your family may also feel hesitant or nervous. Consider identifying the person in your family who knows a lot about your family’s medical history, how your family feels the most comfortable talking with each other, and how much time you might need to set aside to talk. The particular details will vary based on your family, but regardless of how and when you start the conversation, consider approaching the conversation with curiosity, a calm demeanor, an open mind, and compassion.41,42
Before the conversation consider the information you hope to gather, the reason you're asking, and have your questions prepared. This guide with signs and risks could even be a conversation starter: "I found this article about pancreatic and gastric cancer risks and I realized we hadn't discussed if anyone in our family has had this type of cancer before. Would you have some time to talk about it?"41,42
5. What questions could I ask my family to better understand our health history?
- Has anyone in our immediate family been diagnosed with pancreatic or gastric cancer?
- At what age were they diagnosed? How are they doing now?
- Is there any history of genetic disorders in our family that may increase cancer risks?
- Has anyone in our family had genetic testing? What did they learn?42
6. What types of treatment are available for pancreatic and gastric cancer?
Treatment options will vary based on the stage of cancer a person is diagnosed with.43,44 Some common effective treatments for pancreatic or gastric cancers may be surgery, chemotherapy, radiation therapy, targeted drugs, or immunotherapy.43,44 Your health care provider will talk with you about all of your options based on your cancer stage, your unique health risks, and your preferences.
7. Are there any natural options for reducing pancreatic and gastric cancer risks or improving health outcomes?
Risks of developing cancer may be reduced with some lifestyle changes. Some changes may even improve health outcomes after diagnosis like reducing alcohol use, eating a more nutritious and balanced diet, and staying physically active. However, treatment administered by a healthcare provider is the only proven safe and effective way to treat pancreatic or gastric cancer.43,44
Talk to your doctor if you have any concerns about your risks and cancer treatment options, they can help you navigate your options in an informed way.
Sources
- https://www.gicancersalliance.org/resources/gastrointestinal-cancers-an-urgent-need/
- https://www.gicancersalliance.org/wp-content/uploads/2025/07/ActionReport_Final_Digital_7.22_Update.pdf
- https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/aanhpi-cancer-facts-and-figures/aanhpi-cff.pdf
- https://muschealth.org/medical-services/ddc/patients/digestive-organs/stomach-and-duodenum
- https://www.cancer.org/cancer/types/stomach-cancer/about/what-is-stomach-cancer.html
- https://pancan.org/facing-pancreatic-cancer/about-pancreatic-cancer/what-is-the-pancreas/
- https://www.endocrine.org/patient-engagement/endocrine-library/hormones-and-endocrine-function/pancreas-hormones
- https://www.cancer.gov/about-cancer/understanding/what-is-cancer
- https://www.mygutfeeling.ca/what-is-stomach-cancer
- https://www.cancer.org/cancer/types/stomach-cancer/detection-diagnosis-staging/signs-symptoms.html
- https://www.cancer.org/cancer/types/pancreatic-cancer/about/what-is-pancreatic-cancer.html
- https://www.cancer.org/cancer/types/pancreatic-neuroendocrine-tumor/about/what-is-pnet.html
- https://www.cancer.org/cancer/types/pancreatic-cancer/detection-diagnosis-staging/signs-and-symptoms.html
- https://www.cancer.org/cancer/types/pancreatic-neuroendocrine-tumor/detection-diagnosis-staging/signs-and-symptoms.html
- https://www.cancer.gov/about-cancer/causes-prevention/risk/tobacco
- https://www.cancer.org/cancer/types/stomach-cancer/causes-risks-prevention/risk-factors.html
- https://www.cancer.org/cancer/types/pancreatic-cancer/causes-risks-prevention/risk-factors.html
- https://pancan.org/facing-pancreatic-cancer/about-pancreatic-cancer/risk-factors/
- https://www.nyc.gov/site/doh/about/press/pr2022/health-department-releases-new-data-on-smoking-inequities-in-nyc.page
- https://www.cancer.gov/types/stomach/causes-risk-factors
- https://www.cancer.org/cancer/survivorship/be-healthy-after-treatment/nutrition-and-physical-activity-during-and-after-cancer-treatment.html
- https://www.nypl.org/community/resources/food-security
- https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/h-pylori-fact-sheet
- https://www.gastrojournal.org/article/S0016-5085(19)41464-9/fulltext
- https://med.stanford.edu/news/insights/2022/12/stomach-cancer-asians.html
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8375647/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6098981/
- https://pubmed.ncbi.nlm.nih.gov/16033932/
- https://adanews.ada.org/huddles/gum-disease-could-increase-risk-of-stomach-cancer/
- https://www.aacr.org/patients-caregivers/progress-against-cancer/assessing-gum-disease-cancer-risk/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10377021/
- https://pancan.org/pancreatic-cancer-and-the-black-community/
- https://pancan.org/news/taboo-topics-how-to-talk-to-family-about-cancer-risk/
- https://www.dana-farber.org/health-library/family-health-history-conversation-guide
- https://www.cancer.org/support-programs-and-services.html
- https://www.cancer.org/content/dam/cancer-org/cancer-control/en/booklets-flyers/after-diagnosis-a-guide-for-patients-and-families.pdf
- https://www.cancer.gov/about-cancer/coping
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5623134/
- https://pancan.org/pancreatic-cancer-and-the-black-community/
- https://www.cghjournal.org/article/S1542-3565(24)00874-7/fulltext
- https://pancan.org/news/taboo-topics-how-to-talk-to-family-about-cancer-risk/
- https://www.dana-farber.org/health-library/family-health-history-conversation-guide
- https://www.cancer.org/cancer/types/stomach-cancer/treating/by-stage.html
- https://www.cancer.org/cancer/types/pancreatic-cancer/treating/by-stage.html
Heading
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat.


Heading
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat.
The Charles B. Wang Community Health Center is a nonprofit and federally qualified health center offering comprehensive primary care services to all in six convenient locations in Manhattan and Queens seven days a week.








