Taking Charge of HIV Prevention: How Women Can Protect Themselves and their Families
Clinically reviewed by Pearl Tung, DNP

There are many ways to prevent HIV. Understanding risks and prevention options can empower any woman to feel confident managing their own health and the health of their family.
Women Are Impacted by HIV (Human Immunodeficiency Virus)
Any person who is exposed to HIV (Human Immunodeficiency Virus) has some risk of developing HIV, regardless of their sex or gender. A person is exposed to HIV when their blood stream or mucous membrane comes in contact with certain bodily fluids from a person with a detectable HIV viral load. A person may not have any obvious HIV symptoms, so getting regular HIV testing is very important.1

Like other illnesses, the HIV virus impacts certain groups of people differently than others. Often this is due to the systems and structures that prevent many people from achieving their optimal health. Sometimes these structures are obvious, but other times these disparities are difficult to notice. Below we will consider the experiences of people who identify as women broadly, but it is also important to recognize that many women face intersecting risks due to other factors like race, sexuality, immigration history, disability, or something else.2,3

HIV Risks Women May Face
There are biological and social factors that many women face that may increase their risk of exposure to HIV, prevent timely access to medical support for HIV, and present challenges when planning for pregnancy. But there are also steps a woman can take to reduce her risk of getting or transmitting HIV.
Receptive Sex
The receptive partner during anal and vaginal sex has a higher risk of exposure to HIV than their sexual partner. The vaginal and anal walls present a large surface area and any opening in the vaginal or anal walls can be an entry point for the HIV virus.5,7
For women who are engaging in vaginal sex it is important to note that during menopause the vagina produces less lubrication which can increase risk of HIV exposure. Regardless of a person’s age they may consider using condoms to prevent the transmission of HIV. If pairing condoms with a lubricant, be sure to select a water-based or silicone-based lubricant since oil-based lubricants can damage condoms.5,8,9
For women who are engaging in anal sex it is important to get tested for HIV. HIV risk is significantly higher during anal sex than during vaginal sex, yet HIV testing is especially low among women who engage in anal sex. Either an internal (female) or external (male) condom can be used, although external condoms are more effective at preventing HIV during anal sex. When used consistently and correctly, external condoms prevent HIV up to 80% of the time.10,11,12,13,14
Accessing HIV Medications for Treatment and Prevention
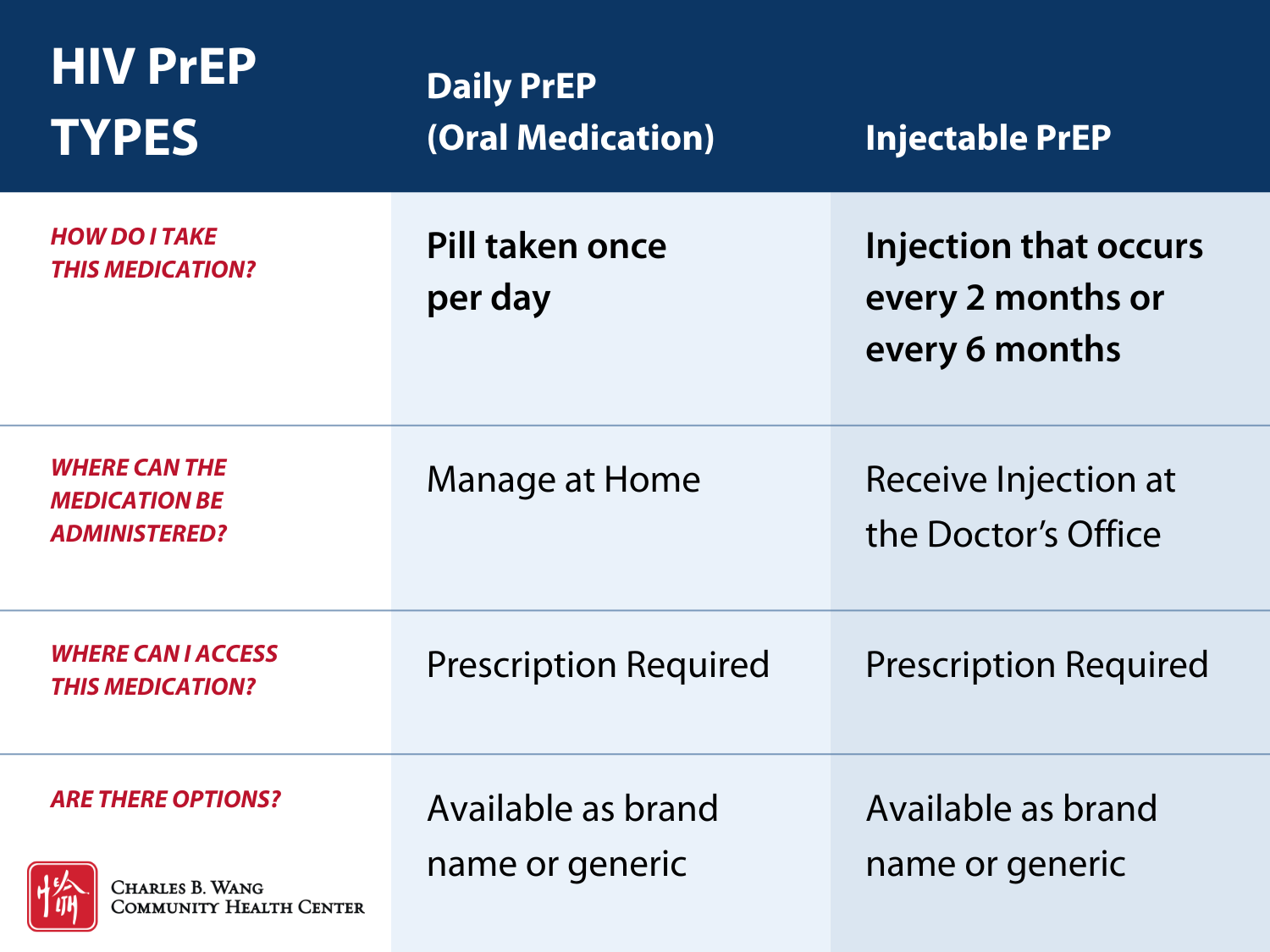
HIV risks can be lowered with certain medications. Pre-Exposure Prophylaxis (PrEP) is a medication that a person can take regularly to prevent HIV. Post-Exposure Prophylaxis (PEP) is an emergency medication that prevents HIV from developing after exposure. Antiretroviral Treatment (ART) is a treatment plan for people who have HIV; it includes medications that a person can take to keep them healthy and prevent HIV transmission to others.
In general, women have slightly lower rates of viral suppression than their male counterparts and significantly lower rates of PrEP use despite potential benefit. The are various reasons that women may be receiving less medical support to manage their HIV risk. HIV medications may not be discussed in their homes or at their doctor’s visits, they may face language barriers, face challenges accessing medical care, mistrust the healthcare system, or they may fear stigma from their families or providers.2,15,16,17
While women may not have control over all of these barriers, understanding your options can support you as you navigate the healthcare system and advocate for your sexual health. If you are considering using HIV medications, think about which HIV medication may work best for you and talk to your doctor about your HIV risks and medical options.
Talking about HIV
Many women may not feel comfortable talking about their sexual health with their provider or their sexual partners. For some, talking about sexual health may feel particularly taboo due to culture, religion, or stigmas in our society. For others, talking about HIV may just be uncomfortable. But starting the conversation about HIV can not only be empowering, it can also be a critical tool for protecting your health.18,19
Talking to a health care provider
While optimal sexual health may look different for everyone, it is still an important part of overall health and well-being. Talking about HIV with a provider may even start conversations about other health topics too, like sexual function, discomfort, healthy periods, or family planning. Your provider may bring up the topic or you may choose to start the conversation yourself. When preparing for a conversation with your provider about HIV, you may first want to prepare a list of questions and concerns by writing them down. Writing down your questions and concerns can help you remember even if you are feeling stress in the moment.19
There are many biases in our society (age, race, weight, sexuality, or disability) that may lead conversations with a provider about sexual health to either not happen at all or be conducted in a way that does not value you or your health. Finding the right provider can be tricky, but your health is worth it. If a provider is not a good fit for you, you do not need to continue receiving care from them. Continue your search for a provider who respects you and your whole health.19
Talking to a sexual partner
Talking to a sexual partner about HIV might feel awkward, but bringing up HIV and sexual health is an important way to care for yourself and your relationships. You might find that preparing for the conversation may empower you to take control of your health and the discussion itself may help you feel more confident navigating your boundaries before having sex.
Consider your own values before talking to a partner:
- What does safe sex mean to me?
- What resources can I access independently to protect my sexual health (condoms, HIV test)?
- What considerations are important for me and my partner to discuss?
It can be helpful to have the conversation before having sex to ensure everyone is on the same page and is able to give informed and enthusiastic consent. During the conversation, you might discuss condoms, HIV testing, and your safe sex boundaries. Remember that it is always an option to say no at any time to sex especially if you do not feel like your health or boundaries are being respected.20
For women living with HIV, notifying a partner of your HIV diagnosis might feel stressful or overwhelming. But talking about it is an important way for us to care for each other’s health and to prevent further spread of HIV. Starting this conversation may also open up new discussions with your partner about caring for each other’s sexual health and well-being, safe sex practices that work for each of you, and the importance of testing and treatment for other STIs. It might help to brush up on your sexual health and HIV knowledge, for example, when a person has an undetectable viral load, the HIV virus is not transmittable through sex. That way you can feel prepared for an open conversation.21
Before having the conversation, you might first consider your safety. If you expect this conversation may not be safe, you might reference your safety plan to determine which strategies you can use in this situation. If you expect this conversation will be safe; consider how, when, and where to tell your partner. In general, the conditions in which you share your HIV status are up to you, however, keep in mind that in some states, there are laws that require a person who tests positive for HIV to inform their sexual partners of their HIV status before having sex, regardless of their viral load.21,22
HIV and Pregnancy
With the current treatment and prevention options available, women living with HIV can live healthy and long lives. Part of this journey may involve a desire to have children. With appropriate treatment and prevention methods, women who are living with HIV can lower their risk of transmitting HIV to their partner or child.
HIV can be transmitted through sexual contact, childbirth, and breastfeeding/chestfeeding. But by choosing a safe conception method and managing their viral load during pregnancy, delivery, and during their child’s early years; women with HIV can have safe and healthy pregnancies and choose to feed their newborn based on their families’ goals.23
The most important way to prevent HIV transmission during the pregnancy journey is by starting and maintaining appropriate HIV treatment. When following an appropriate treatment regimen, a woman’s viral load can become undetectable. When a person’s viral load is undetectable, they cannot transmit HIV through sexual contact and the risk of transmitting HIV to their child during pregnancy, childbirth, and breastfeeding is less than 1%.23,24
Gender Based Violence
All women deserve to have safe and healthy relationships and express their sexuality safely. However, it is an unfortunate reality that many women and girls may face intimate partner violence (IPV) or sexual violence. Abuse and assault are never the survivor’s fault.
Gender based violence can have serious health consequences. One serious health consequence is an increased risk of HIV. Despite these risks, women who have concerns about preventing HIV due to gender based violence still have options.22,25
Anyone who has experienced a sexual assault may consider talking to a medical provider as soon as possible. A medical provider can assess immediate health concerns, like injuries or sexually transmitted infections (STIs), and connect a person to resources. For individuals at risk of HIV, their doctor may talk to them about Post-Exposure Prophylaxis (PEP). PEP is most effective when taken as soon as possible after the exposure and is only effective if taken within 72 hours.26,27
Some women may be facing ongoing abuse or assault, or they may not be in control of their sexual health for many reasons. PrEP is a medication that a woman can use independently and discreetly to prevent HIV. PrEP can even be administered as an injectable medication at the doctors office; depending on the medication, a person can be protected from HIV with an injection every 2 months to just twice a year.22
If you have experienced abuse or assault, remember it is not your fault. If you need assistance or support, you are not alone, and resources like the National Domestic Violence hotline can help.
Protect Yourself – Know Your Options
Every person who is sexually active can take an active role in managing their sexual health. There are many ways a person can prevent getting or transmitting HIV, and many HIV prevention methods can be used in combination. Consider which methods work best for your life, that you feel confident using, and that you can use consistently. Talk to your doctor about your concerns and your risks, and they can help you plan for the methods that will work best for you.
- Minimizing Risk of HIV Exposure
To reduce the risk of HIV transmission during sex, a person can consider: using barrier methods like internal or external condoms consistently and correctly, choosing sexual activities that have a lower risk of transmitting HIV, or abstaining from sex – remember that consent is reversible, you can always say no, even to something you may have consented to in the past.
- HIV Testing – Know Your Status
HIV testing is lifesaving. There are many options for accessing confidential and low or no-cost HIV testing options; rapid HIV tests can even provide results within 30 minutes. Testing is the only way to know your HIV status. When you know your HIV status, you can take steps to maintain your health and protect your loved ones.
- Talking to your Doctor about HIV Medicines
HIV prevention medications are an option for protecting yourself and your family from the health risks of HIV, and they may be a good fit for you. These medications can be used to prevent HIV proactively (PrEP) or as an emergency medication to prevent HIV after exposure (PEP). Talk to your doctor about HIV medicine if you think you may benefit from PrEP or PEP.
HIV treatment medicines can also prevent HIV transmission and protect your health (ART). Treatments for HIV are very effective with little to no side effects. If you have been diagnosed with HIV, starting treatment with HIV medicine as soon as possible is the best way to keep yourself and your partners healthy.
Women’s Health at the Charles B. Wang Community Health Center
At the Charles B. Wang Community Health Center, we are committed to empowering women and providing the personalized health care and support that all women deserve. From dental health to sexual health, women can access services to care for their whole selves with providers who speak their language and value their health.
If you would like to start the conversation about HIV, providers in our Internal Medicine and Obstetrics & Gynecology departments can talk with you about your HIV risk, discuss preventative medications like PrEP, administer confidential and low cost HIV testing, and connect you to other low or no-cost HIV prevention resources like condoms. For women with specific sexual health or reproductive health concerns, our Obstetrics & Gynecology providers care for women of all ages, during any stage of life.
- Schedule an appointment with an Internal Medicine Provider
- Schedule an appointment with an Obstetrics & Gynecology Provider
Charles B. Wang Community Health Center accepts most major insurance plans and offers fee discounts for people without insurance based on family size and income. Services are provided regardless of a patient's ability to pay or their immigration history. CBWCHC offers care at five convenient locations in Manhattan and Queens as well as virtual visits, so you can feel confident accessing care on your terms.
FAQ:
1. What is HIV?
HIV is a virus. Viruses are a very common type of infectious organism that cause illnesses in humans. Some viral infections (like the common cold) go away on their own while other infections (like HIV) require treatment. Most viral infections do not have medical cures, so prevention is very important.
When a person has HIV, the HIV virus primarily attacks their immune cells (specifically T-cells). As the HIV virus continues to attack the immune system, it becomes more and more difficult for the body to protect itself from other infections or diseases. Without treatment, the HIV virus may continue to damage the immune system until the body can no longer fight severe infections or cancers. When a person progresses to this late stage of HIV they may be diagnosed with Acquired Immunodeficiency Syndrome (AIDS).28
HIV treatment reduces the amount of the HIV virus in the body. When a person follows an HIV treatment regimen, they can reduce the amount of HIV in the body to a level that is so low it is undetectable. When a person’s viral load is low, the immune system is less likely to be affected by the virus. This means they are less likely to get sick, they are less likely to develop AIDS, and they are less likely to transmit HIV to another person.
2. Do We Have Any Evidence that HIV Impacts Certain Groups Differently Than Others?
- In New York City in 2023 only 35% of sexually active women had heard about PrEP.6
- About 1 in 4 Asians living with HIV and 1 in 4 Native Hawaiian/other Pacific Islanders living with HIV did not receive medical care for their HIV in 2023.32
- In the US, more than 1 in 5 transgender women are living with HIV.29
- In 2022, the number of Black women diagnosed with HIV was eight times higher than their white female counterparts.30
- Women who are assigned female at birth are most likely to be exposed to HIV during sex with a male partner.2,5
- Among all people living with HIV at the end of 2022, women had one of the lowest rates of viral suppression (64%).31
3. How Can I Learn More About PrEP?
Talking to your doctor can be a good place to start when you are considering PrEP options. They can help you identify your HIV risks and get a better understanding about which medications may be best for you and your health history.
If you would like to learn more about different PrEP medications before speaking with your provider, these resources below have some additional details that can guide your discussion with your provider. Medication details may change over time, so be sure to follow up with your doctor to get the most accurate and up-to-date information.
4. What is a safety plan?
In the case of intimate partner violence or abuse, an important step a person can take for their own safety is to develop a safety plan. A person can develop a safety plan regardless of their interest, readiness, or ability to leave a relationship. A safety plan helps you think through your physical, sexual, digital, and emotional safety. You can find safety plan resources online through National Domestic Violence hotline.33
5. What is Gender Based Violence?
Gender based violence (GBV) is a term that refers to a type of harm that is perpetrated based on someone’s sex or gender. National statistics have shown that in their lifetime, over 1 in 3 women report some form of IPV, more than 1 in 2 transwomen report some form of IPV, and more than 1 in 2 women report some type of sexual violence.34,35
Sources:
- https://www.cdc.gov/hiv/causes/index.html
- https://www.cdc.gov/hiv/data-research/facts-stats/women.html
- https://www.thewellproject.org/hiv-information/why-race-matters-women-and-hiv
- https://www.unaids.org/en/resources/fact-sheet
- https://womenshealth.gov/hiv-and-aids/women-and-hiv
- https://www.nyc.gov/assets/doh/downloads/pdf/ah/women-hiv-infographic.pdf
- https://www.thewellproject.org/hiv-information/hiv-transmission
- https://www.thewellproject.org/hiv-information/older-women-sex-and-hiv
- https://www.nia.nih.gov/health/sexuality/sexuality-and-intimacy-older-adults
- https://stanfordhealthcare.org/medical-conditions/sexual-and-reproductive-health/hiv-aids/causes/risk-of-exposure.html
- https://www.thewellproject.org/hiv-information/talking-your-partner-about-condoms
- https://www.cdc.gov/condom-use/resources/internal.html
- https://www.health.state.ny.us/diseases/aids/consumers/condoms/faqs.htm
- https://www.aidsmap.com/about-hiv/do-condoms-work
- https://www.thelancet.com/journals/lanam/article/PIIS2667-193X(24)00065-6/fulltext
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5708581/pdf/nihms915240.pdf
- https://doi.org/10.1089/apc.2025.0006
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11319820/pdf/cureus-0016-00000066723.pdf
- https://www.cdc.gov/stophivtogether/talk-hiv/index.html
- https://www.plannedparenthood.org/learn/stds-hiv-safer-sex/safer-sex/how-do-i-talk-my-partner-about-safer-sex
- https://www.thewellproject.org/hiv-information/disclosure-and-hiv
- https://www.thewellproject.org/hiv-information/violence-against-women-and-hiv
- https://www.thewellproject.org/hiv-information/getting-pregnant-and-hiv
- https://www.thewellproject.org/hiv-information/getting-pregnant-and-hiv
- https://womenshealth.gov/hiv-and-aids/women-and-hiv/violence-against-women-and-hiv-risk
- https://rainn.org/getting-medical-help-after-sexual-assault/protecting-your-health-after-sexual-assault/
- https://www.nyc.gov/site/doh/health/health-topics/post-exposure-prophylaxis-pep.page
- https://womenshealth.gov/hiv-and-aids/hiv-and-aids-basics
- https://www.hrc.org/resources/transgender-people-and-hiv-what-we-know
- https://stacks.cdc.gov/view/cdc/156513
- https://www.amfar.org/about-hiv-aids/hiv-aids-in-the-us/
- https://www.cdc.gov/hiv/data-research/facts-stats/race-ethnicity.html
- https://www.thehotline.org/plan-for-safety/
- https://www.thehotline.org/stakeholders/domestic-violence-statistics/
- https://transequality.org/sites/default/files/docs/usts/USTS-Full-Report-Dec17.pdf
Heading
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat.


Heading
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat.
The Charles B. Wang Community Health Center is a nonprofit and federally qualified health center offering comprehensive primary care services to all in six convenient locations in Manhattan and Queens seven days a week.








